
Regarding the worldwide crisis brought about by governments' response to the SARS-CoV-2 virus, for nine months the Reader has kept to our mission of providing news and information beyond what is delivered by both local and national corporate media. Alternative information and viewpoints are what we do, and COVID-19 is no exception. In fact, because of its importance to our bio-future and personal freedoms, understanding COVID-related issues deserves as deep a dive as we can muster.
[Dec 11, 2020: Here are the counties' answers to the Reader's questions: https://www.rcreader.com/commentary/dr-katz-answers-11-covid-questions]
By now, readers should be understandably concerned over the Herculean efforts by health authorities, so-called journalists, and social engineers (Facebook, Twitter, Google, and YouTube) to censor any skepticism surrounding SARS2-CoV-2 (virus)/COVID-19 (disease) as a lethal pathogen threatening humans.
After nine months of research, clinical observation, and accumulated data analysis of millions of people and outcomes worldwide, highly credentialed medical professionals and scientists emphatically disagree. Rational disagreement is often what science requires, and in the case of COVID-19, potentially providing game-changing positive discovery toward ending our collective misery enduring lockdowns, mask-wearing, and continued isolation.
Rather than standing at odds with these growing numbers of legitimate skeptics, equally convicted health authorities need to participate by answering more probing questions that persist. There may be undisclosed answers for why COVID-19 is considered to be a pandemic-level disease, even though its epidemiology suggests it is undeserving as it is not substantially different than common flus and/or cold strains (many of which are also coronaviruses) for most people.
Again, tens of thousands of medical personnel in practice, academia, and research have expressed grave concerns over inconsistencies in diagnoses, data collection, and treatments; flawed diagnostic tools; contradictions in otherwise traditional protocols for peer review and scientific analysis; and a growing compendium of incoherent conclusions inevitably parroted by corporate media and social engineers to influence public acceptance of extreme mitigation policies.
Yet the large body of science that underpins growing skepticism, by the world's medical community and public at large, is rarely addressed by any of the designated “trusted voices” such as Dr. Anthony Fauci or Dr. Deborah Birx. And therein lies the deeper problem. This lack of transparency and defiant unwillingness to confront legitimate and rational skepticism, even going so far as to systematically censor it, is a neon red flag affirming skeptics are on to something important.
This same dynamic is bearing out here in Scott County, Iowa, and Rock Island County, Illinois. On October 27, 2020, both counties' Health Department officials held a presser to correct “misconceptions” in the community about COVID-19. There was genuine anticipation for questions and confusion to be cleared up relative to COVID-19, such as the PCR tests' reliability in diagnosing a disease via detecting a partial target viral fragment; or why the fixation on increased cases are now the basis for threat assessment relative to COVID-19; or why the number of deaths are no longer the foremost measure of lethality for COVID-19, as it has been for every other infectious disease for centuries? Alas, much was left unaddressed. To the health departments' great credit, they are posting the recording of their pressers and you can watch the October 27 presser at the county website, here, or in the video embed below. And, you can read their effort to correct misconceptions at the end of this article where the news release that went out after the presser is published. This effort is very appreciated.
In the spirit of cooperation and collaboration, the Reader has prepared and delivered questions as a means of engagement with our local health authorities requesting them to kindly respond in writing. We will publish their responses for Quad Citizens, hopefully bringing clarity, informed understanding of the relative risks, and perhaps even alleviate dread, simultaneously re-energizing confidence in community health stewardship. Interest in topics and issues can be enriched by our public servants' responsiveness to questions and concerns, especially as our local “trusted voices.”
COVID-19 Questions
A “case” of an infectious disease has traditionally meant that a person is infected with enough virus (viral load) to cause symptoms of the disease, as well as to infect others at this time. Ninety percent of people testing positive for SARS-CoV-2 have no symptoms – are asymptomatic – so by definition do not have enough virus present to cause COVID-19 disease, and are therefore not contagious, either. One of the FDA's parameters for COVID-19 Testing Guidelines warns testing providers to verify any viral detection with clinical confirmation of symptoms before making an affirmative diagnosis a.k.a. "a case," indicating that the PCR test alone cannot diagnose disease because it does not detect the amount of virus.
1) How are these guidelines being followed when testers and providers are diagnosing asymptomatic people that test positive as "cases"?
The newest COVID-19 controversy concerns the validity of the RT-PCR Test as a reliable diagnostic tool due to the cycle thresholds being set too high to accurately confirm the presence of the target viral fragment, and often resulting in false positives based on other material present, such as dead virus. Dr. Anthony Fauci, in an interview with This Week in Virology (July 16, 2020), describes the PCR test's weakness: “If you have a cycle threshold of 35 or more, the chances of it being replication competent are miniscule.” He further explains that “you can almost never culture virus from a 37, 38, even a 36 cycle threshold … you have to say it's just dead nucleotides.” The cycle threshold for most PCR tests range from 37-45, with LabCorp averaging btw 38-40 cycle thresholds, according to the FDA.
2) By what criteria do you confidently diagnose asymptomatic people with COVID-19 who test positive at those higher 38-40 cycle thresholds, knowing the amplification is too high to be definitive for the presence of SARS-CoV-2 virus, let alone enough to cause an actual case of COVID-19 disease?
Even at a lower cycle threshold of 29-33, a positive test result indicating the presence of the target viral fragment does not indicate how much of the virus (viral load) is present in the body for a definitive diagnosis of COVID-19 disease without further clinical observation.
3) And if the disease cannot be confirmed as present due to no symptoms, how can these asymptomatic people be classified as cases, and/or contagious?
4) Do you contact trace from asymptomatic people who test positive with cycle thresholds higher than 35, and if so, what is your justification if the originating viral detection was too low to replicate, meaning not contagious?
5) What percentage of reported "cases" are from people who were contact traced and presumed to be positive, but not actually tested?
For the remaining 10 percent of people who are symptomatic and confirmed with both positive testing and clinical observation, the recovery rate is 99 percent for patients under 70, and 94 percent for patients 70 and older, according to the CDC. In the same report, most symptomatic patients experience a range of symptoms, most often mimicking a harsh flu or severe cold. COVID-19 hospitalizations were consistently due to underlying conditions, not COVID alone.
6) When reporting the number of hospitalizations, how do you differentiate between patients suffering from similar illnesses such as flu or respiratory conditions, causing COVID-19 to be subordinate to these often more serious conditions?
The CDC has confirmed in its recent report on mortality (using actual data versus predictive models) that the survival rate for those with COVID-19 is 99 percent for everyone under 70 years of age, and 94 percent for those 70 and older. It is well documented that COVID-19 impacts our elderly, almost always with two or more comorbidities. Yet health officials have chosen to concentrate resources for assessment and mitigations on 99 percent of the population to protect the vulnerable 1-percent demographic.
7) What is the rationale for this strategy? Please be specific.
The CDC also recently reported that deaths “from” COVID-19 were substantially less than deaths “with” COVID-19. The report underscored the majority of deaths with COVID-19 had comorbidities that were the primary causes of those deaths. Yet comorbidities are rarely mentioned by health authorities when reporting COVID-19 deaths.
8) Why is this significant comorbidity data omitted from news releases/reporting on a patient dying from COVID-19, when it would otherwise be most useful in assessing risk from SARS-CoV-2?
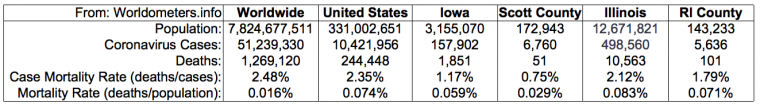
Number of deaths has been the primary measure of lethality of an infectious disease for centuries until COVID-19. Today, the constant crisis is perpetuated by the number of rising cases. Yet even though the number of cases is rising, the number of COVID-19-related corresponding deaths has not. This is consistently true worldwide. According to the CDC, deaths due to COVID-19 are infinitesimal as a percentage of the global population, bringing into question, by definition, the status of SARS-CoV-2 and COVID-19 as a true pandemic. (See chart below.)
9) Why are deaths no longer the leading indicator of lethality for COVID-19?
In the October 27 presser, county health officials stated "Because we do not know exactly how someone’s body and immune system will respond to the coronavirus, 100 percent of people are at risk of dying from COVID-19." Volumes of evidence are to the contrary.
10) How can health officials lump all people into a risk category for contracting any disease and dying based solely on the vast “unknown” regarding immune systems?
11) If there are no excess deaths, or threats of death from COVID-19 for 99 percent of the population, what precisely is the justification for the extreme mitigations? In other words: How does shuttering businesses, closing schools, limiting access to health care (especially to provide care for patients with a single illness that has far less risk of death than many other patients whose conditions include far greater mortality rates), wearing masks for prolonged periods, and isolating people from one another indefinitely, measurably prevent 1 percent of the population from harm due to COVID-19? Please be specific.
Thank you for your participation. We look forward to your responses. We hope this is a new path for active civic engagement and robust communication. After all, as you thoughtfully remind us, we are in this together.
Quad Cities COVID-19 Coalition
FOR IMMEDIATE RELEASE
October 27, 2020
Current COVID-19 case count
Scott County – Total of 4,619
Total deaths in Scott County: 41
“Since our last press briefing, four additional COVID-19 related deaths of Scott County residents been reported,” said Amy Thoreson, deputy director, Scott County Health Department. “One was an older adult age 61-80; and three were elderly adults greater than age 80. We express our sympathies to the family and friends of these Scott County residents. It is always hard to report deaths of members of our community, and we have seen too many COVID-related deaths reported this month alone.”
Rock Island County – 54 new cases since Monday; total of 4,251
Currently in hospital: 25
Total deaths in Rock Island County: 101
Newly reported death: A man in his 60s who died at a long-term care facility
“Sadly, we are reporting the county’s 101th COVID-19 death,” said Nita Ludwig, administrator of the Rock Island County Health Department. “We offer our sympathies to her family and friends.”
Today’s call
A video recording of today’s media briefing can be found at https://www.scottcountyiowa.
Scammers pretending to be contact tracers
Remarks from Janet Hill, chief operating officer, Rock Island County Health Department
With the recent surge of COVID-19 cases, our contact tracers are busy. Unfortunately, so are scammers. Our contact tracers are calling to break the chain of infection in our communities. We need you to pick our calls and answer our questions.
Contact tracing is a basic and free public health infection control measure, and it is confidential. Your contacts only will be told that they were exposed to the virus — they will not be told your name.
We will never ask you or any of your contacts for financial information, payment for services or your Social Security number. Anybody who does is a scammer. Please note the number that called you and alert your local police department.
Our contact tracers are working at the Rock Island County Health Department. They are using a statewide data system that calls from 312-777-1999. Even though it’s a Chicago number, Rock Island County Health Department workers are calling you. Please pick up. We also might be calling from a health department phone. Those numbers start as 309-558. We also may call from a health department cell phone. Those numbers start as 309-737.
In Scott County, contact tracers will call from numbers that start 563-326.
Correcting misinformation
Remarks from Nita Ludwig, administrator, Rock Island County Health Department
As we have said from day 1, the novel coronavirus is just that – novel, meaning new. We have watched in real time as our public health and health care systems have learned more about the virus and associated COVID-19 illness nearly daily.
We never expected ourselves to be in a pandemic of global proportions. We know it would be easier to write off what we hear about COVID-19 as untrue or inflated. It would surely be easier to live our day-to-day lives if a pandemic wasn’t looming.
For these reasons, we hear many misconceptions shared about the virus, sometimes in an effort to downplay it with the hope of living our lives with fewer restrictions at this time. We want to take today’s briefing to help describe the misconceptions and provide accurate information.
Misconception #1: Most people with COVID-19 don’t get very sick, so it’s not a big deal.
· First, it is hard to get a handle on how many people have COVID-19.
· Some individuals may have it and don’t know it.
· Some individuals may have such mild symptoms that they don’t consider COVID-19 as the cause and therefore don’t get tested.
· Then we still have the group of individuals that we know have COVID-19 because they tested. This group varies across a spectrum, from individuals with very mild symptoms to more severe symptoms to individuals with very serious symptoms requiring hospitalization.
· Of those individuals with more serious illness, we are hearing reports of individuals having lasting lung issues, long past their actual recovery from the virus. Others end up on ventilators in the ICU. And there are others still that die as a result of their illness.
· Remember, individuals that end up contracting COVID-19 will end up falling somewhere on that spectrum in terms of symptom severity.
· There is no magic indicator of whether someone will have mild illness or more severe illness.
· As the virus continues to spread, it puts individuals who are more vulnerable (such as those who are older or have underlying heath conditions) at greater risk of catching the virus and experiencing severe illness.
Misconception #2: About 99.9% of people aren’t at risk of dying from COVID-19
· This was a statement that we read in our community recently.
· Because we do not know exactly how someone’s body and immune system will respond to the coronavirus, 100% of people are at risk of dying from COVID-19.
· You can’t turn on the news without hearing a story of a healthy young adult succumbing to the virus. In our own community we have experienced deaths of individuals from their early 30s to older than 80.
· The virus itself does not discriminate.
Misconception #3: The PCR test (test used to identify current infections of COVID-19) doesn’t really even tell us who could currently spread the virus to others.
· The PCR test is the current test used to determine if an individual is currently infected with the SARS-CoV-2 virus, also known as the coronavirus.
· It detects if the genetic material of the SARS-CoV-2 virus, the RNA, is currently present.
· The test is considered to be very reliable.
Misconception #4: This whole virus has been blown out of proportion and will be over/out of the news after the presidential election.
· Since March 21, when the first case of COVID-19 was confirmed in a Scott County resident and March 22 for a Rock Island County resident, contact tracers from both health departments have conducted in-depth interviews with more than 90% of the 8,000 individuals that have tested positive in our counties.
· These are individuals who voluntarily tested based on showing signs of illness or being in close contact to someone with COVID-19.
· These people are real. Their stories are real. Their symptoms are real. This virus is real.
· While politics may dictate the federal response to this virus, this virus will not magically disappear after the election.
· I can guarantee that after the outcome of the presidential election is decided, we will continue to have spread of the virus, people will continue to show symptoms of the virus, people will continue to test positive for the virus, and we will continue to contact trace to help stop it.
More corrections to misinformation
Remarks from Amy Thoreson, deputy director, Scott County Health Department
Misconception #5: We should just let everyone get COVID-19 and then we wouldn’t have to worry about it anymore.
· Herd immunity is a real thing, and in this case, a real scary thing.
· Herd immunity occurs when a high percentage of the community is immune to a disease (either through immunization or prior illness).
· Attempts to reach ‘herd immunity’ through exposing people to a virus are scientifically problematic and unethical.
· Letting COVID-19 spread through populations of any age or health status will lead to unnecessary infections, suffering, and death. Much of the burden of infections, suffering, and death would be disproportionately borne by those who are most vulnerable in our community: older adults, individuals with underlying health conditions, low-income and minority individuals in front-line work who are more at risk for exposure to a virus that is spreading.
Misconception #6: If I have already had COVID-19, I don’t have to wear a mask.
· Each day we learn more about this new virus that is spreading in our community.
· Current data tells us that COVID-19 antibodies can last in an individual that was infected with the coronavirus for a short amount of time, although we do not know how long.
· This means that over time, the individual can once again be at risk of being infected by the coronavirus if they come into contact with an individual who is currently infectious.
· Conversely, the individual can also once again become infected with the virus and possibly spread it without even knowing they are infected.
· It remains very important for all individuals to wear a mask, socially distance, and stay home when they are sick to help reduce the spread of this virus.
Misconception #7: I don’t have a fever so I must not have COVID-19.
· In case you haven’t noticed, the symptoms of COVID-19 are vast and similar to symptoms of a number of respiratory illnesses and some gastrointestinal illnesses, too.
· Unfortunately, there is no stand-alone symptom that definitively tells someone they have COVID.
· In talking with our contact tracers that interview all individuals who are positive for COVID, many actually do not have a fever. Their symptoms may be as mild as mimicking seasonal allergies or a minor sinus infection.
· The only way you will know if you have COVID is to get tested.
· Many employers and other group settings are checking temperatures upon entry. This isn’t because fever is a tell-all for COVID – it’s because it is one symptom that can be monitored externally. We encourage all who are monitoring temperatures also to ask if individuals are also experiencing any other COVID-19 symptoms: fever, cough, shortness of breath, trouble breathing, new loss of taste or smell, diarrhea, severe headache, or muscle aches.
· Individuals experiencing any symptoms should stay home and consider getting tested.
Misconception #8: I’m not worried about catching COVID-19 at a gathering (family gathering, wedding) because people won’t come if they’re sick.
· Boy, do we wish this was true.
· At these types of events, you could run into any of the following:
o An individual that has COVID and doesn’t know it. (asymptomatic)
o An individual that has such mild symptoms that they don’t consider COVID-19 as the cause and go about his or her business.
o An individual that knows they have COVID and attends anyway
· Unfortunately, we have heard too many stories of individuals knowingly interacting when they have had a positive COVID-19 test
· You can know someone, love someone, trust someone and that person could still have COVID and not know it.
· Our first recommendation is to not participate in these types of gatherings, especially as they head indoors, because the level of risk of spread of COVID-19 is pretty high.
· If you must attend a gathering, wear your facemask at all times. And keep at least 6 feet of distance between yourself and others who don’t live in your household.
We know you’re over this all. We couldn’t agree with you more. We are tired, we are feeling defeated, and we don’t have a clear picture of how and when things will change. But this virus isn’t done with us. We are at a dangerous point where the willingness of our community to respond is waning just as our level of risk of the virus is increasing. The risk someone has of catching COVID in the community is so much higher now than it was when we were locked down back in March in April because the number of cases is so much higher. This virus doesn’t care how run down we feel and how frustrated we are. All it needs to spread is close contact and no face coverings. And gatherings such as Thanksgiving and other winter holidays.
The time to act is now.










